Left Navigation - Cardiac Catheterization
Cardiac Catheterization
Catheters have transformed heart disease care, replacing large incisions with minimally invasive procedures that offer less pain, lower risks and faster recovery.
At Stony Brook University Hospital and Stony Brook Southampton Hospital, our skilled interventional cardiologists use state-of-the-art facilities to perform a wide range of diagnostic and therapeutic catheter-based procedures. As a recognized leader in this field, our experts offer care around the clock. Our catheterization labs are available 24/7 to provide emergency procedures when every second counts.
Conditions Treated
Cardiac catheterization is a minimally invasive procedure used to diagnose and treat a range of heart and blood vessel conditions. The procedure is used to:
- Diagnose heart problems, including issues with heart valves or heart muscle
- Find and treat blockages in the coronary arteries using balloons and/or stents (angioplasty)
- Treat conditions in other arteries, such as:
- Carotid arteries (leading to the brain)
- Renal arteries (leading to the kidneys)
- Leg arteries
- Treat congenital heart defects and valve problems
Benefits of Cardiac Catheterization:
- Minimally invasive — no large incisions
- Usually done as an outpatient procedure
- Less pain and faster recovery compared to open-heart surgery

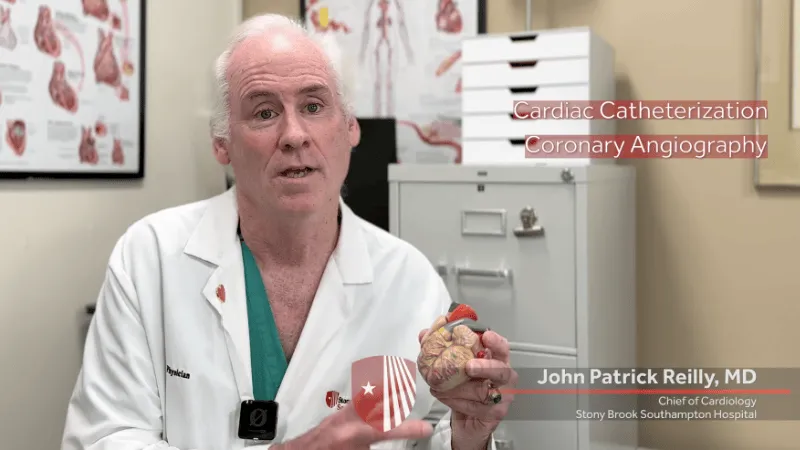
Cardiac Catheterization: How Minimally Invasive Procedures Are Transforming Heart Care
Thanks to advances in technology and technique, diagnosing and treating heart disease have never been more precise and effective. One of the most impactful developments in this field is cardiac catheterization, a minimally invasive procedure that allows physicians to access the heart through a tiny incision.
Cardiac Catheterization Services
Our highly skilled physicians will work with you and your primary care physician to accurately diagnose your condition and determine the best course of treatment for you. Our services include:
- Cardiac catheterization and coronary angiography
- Angioplasty
- Stenting
- Intravascular ultrasound
- Laser angioplasty
- Balloon valvuloplasty
- Percutaneous Left Ventricular Assist Device placement
- PFO/ASD closure
- Impella
Read Our Patient Stories
Meet Scott Mandia: A Cardiac Catheterization Found Heart Disease

The last thing fitness buff and avid runner Scott Mandia, then 55, had on his health radar was heart disease. But, as Scott would soon learn, that was all about to change...
Meet Jodi Kennedy: Overcoming a Widow Maker Heart Attack

A second opinion at Stony Brook changed everything for Jack Brady, uncovering severe coronary blockages that required a life-saving quadruple bypass. Now back to his active lifestyle, Jack is grateful for the care that gave him a second chance and hopes to inspire others to prioritize their heart health.
Our Team
Our award-winning interventional cardiology team is made up of experienced specialists focused on your recovery. We create a personalized treatment plan, emphasizing coordinated care with your cardiologist and primary care physician, and combine decades of experience, advanced research and state-of-the-art facilities to ensure the best possible outcomes and patient experience.
What to Expect During Cardiac Catheterization
Cardiac catheterization is a common, nonsurgical procedure used to check for blockages in the arteries that supply blood to your heart. It also helps doctors see how well your heart pumps, the size of its chambers and how your valves are working.
During the procedure, a small, flexible tube (catheter) is inserted into a blood vessel, typically your groin, and guided to your heart. Doctors take blood pressure measurements and X-ray images (angiograms) to get a clear picture of your heart’s health.
Here’s what you should know before, during and after a cardiac catheterization.
Pre-Admission Testing
Once your physician determines that you need a cardiac catheterization, various tests will help properly assess your condition prior to the procedure. You may have already done tests before your referral; however, Stony Brook Heart Institute staff may request additional testing.
The following are necessary prior to scheduling a catheterization:
- A history and physical examination by a cardiologist or an accredited nurse practitioner
- An electrocardiogram (EKG)
- Blood tests
Other tests may be requested including:
- Exercise tolerance test (treadmill test)
- Echocardiogram (an ultrasound study)
- Gated blood pool scan (nuclear scanning of your heart)
- Chest X-ray
Preparing for Your Cardiac Catheterization
- Do not eat food or drink (except a few sips of water with medication) after midnight.
- Continue to take medications on your prescribed schedule. Medications such as Coumadin, diuretics, insulin and oral diabetic medication will require individual review by your physician.
- The afternoon before your procedure, a nurse from the Cath Lab will contact you to provide additional instructions and let you know when to arrive. Please use this opportunity to address any questions or concerns about your procedure.
- Arrive in the Cath Lab at your designated time. A family member or friend may accompany you.
- It is not necessary to bring anything with you except personal toiletries and medications you may need. Please do not bring any valuables or jewelry. Wear comfortable clothing and walking shoes. You are allowed to bring a book or other diversion to help pass the time in case of delays.
- When you arrive at the Heart Institute, a receptionist will greet you and notify the team that you have arrived. As your procedure time nears, a nurse will ask you to change into hospital attire. You are then brought into the pre-procedure holding area.
For patients in the hospital, a Cath Lab physician will visit you the evening before your procedure to discuss what to expect. We recommend using this time to ask any questions you may have. You will also be asked to sign a consent form.
Adjustments may be made to your prescribed medication routine, and an IV will be inserted. You will not be able to eat or drink (except water with medications) after midnight. Your nurse will ensure that you are properly prepared.
During Your Cardiac Catheterization
- A nurse will check your vital signs, review your medical history and insert an IV.
- You’ll meet the doctor, who will explain the procedure and answer any questions.
- A mild sedative will help you relax.
- You’ll lie on a table with monitors and cameras around you.
- The insertion site (usually your groin or arm) will be cleaned, numbed and prepared.
- A small tube (catheter) will be guided to your heart to take measurements and X-ray images.
- A special dye will be used to highlight your arteries and heart chambers. You may feel a warm or flushed sensation briefly.
- Your physician will review the results with you and discuss next steps.
- If an intervention is needed, it may be performed during the same procedure, depending on the severity and location of the blockage.
Post-Cardiac Catheterization Care
- Rest: Stay in bed for four to six hours and lie flat. Avoid bending your knee.
- Drink fluids: This helps flush out the dye. A nurse will assist you if needed.
- Watch for symptoms: Tell the staff if you feel chest pain, shortness of breath, dizziness or discomfort near the insertion site.
- Going home: Have someone drive you home and stay with you overnight. Rest and limit activity to light tasks the next day.
Frequently Asked Questions
An angiogram is a picture of your arteries obtained under X-ray using a contrast agent. Angiograms of the heart arteries (coronaries) are obtained by a procedure called cardiac catheterization. A large artery either in the leg at the groin or the wrist is entered with a small catheter similar to an IV. Catheters (thin hollow tubes) are then passed up the large aorta to the heart, and pictures of the heart arteries are obtained by administering contrast under X-ray.
Mild to moderate sedation is given to patients, taking in mind the patient and procedure risks, to alleviate pain and anxiety. Local anesthesia is given at the site of the artery in the groin or wrist to minimize pain. Once the artery has been accessed, the procedure after this is usually without discomfort.
If a blockage is determined to be the cause of symptoms, then through the catheterization procedure a small balloon and a stent can be delivered into the artery to push the blockage out of the way to allow unobstructed blood flow. Some blockages, depending on the site, severity and extent might require an evaluation for a surgical procedure called a coronary bypass that re-routes blood around the blockage using bypass graft veins or arteries.
No. But all blockages need to be treated with medical management that includes appropriate risk factor modification, such as smoking cessation, diet, weight management, exercise, stress reduction as well as treatment of hypertension, high cholesterol and diabetes. Medications prescribed, such as aspirin and cholesterol-reducing agents like statins, help to minimize the occurrence of heart attacks, reducing progression of blockages as well.
Stents are fine metal tube-like mesh wire scaffolds delivered into the artery over a balloon that pushes the blockage outward and holds the artery open (scaffold) once the balloon is removed. Over time a lining forms over the stent and the stent becomes part of the artery. Stents do not collapse. However, in a small percentage of patients, the same lining that forms can grow like scar tissue and block the flow of blood, which might require repeat treatment. Stents have been found to be safer and more durable than other invasive artery-opening methods available.
Drug-coated stents are similar to regular stents but have a drug coating on their surface. This drug will be delivered to the wall of the artery to prevent the development of scar tissue buildup and the need for repeat artery-opening procedures. There are different types of such stents, and this is constantly improving with newer developments.
Stents being metal are foreign to the body. Until they get a lining that covers them, they are exposed to blood. This lining might take a month to develop with regular stents or six to 12 months with drug-coated stents. Platelets are blood cells that can clump together on the stents, form a clot and abruptly and dangerously block the stents. Like aspirin and Effient (prasugrel), Plavix (clopidogrel) belongs to a group of anti-platelet drugs that can prevent this clumping from happening, and are extremely important to take diligently once a stent is placed. Do not stop taking these medications without speaking to your cardiologist.
Yes. Stents can be placed in other arteries for symptomatic blockages, such as the arteries that provide blood flow to the brain (carotid arteries), the kidneys (for severe uncontrolled hypertension and kidney failure) or the legs (for incapacitating pain while walking or non-healing wounds). A careful discussion with your doctor is needed of risks, benefits and alternatives before such treatment is undertaken.
These stents are MRI compatible up to 3 teslas. The magnet in an MRI machine is rated using a unit of measure known as a tesla. Some of today's MRI machines are stronger than 3 teslas. The various stent companies have laid out certain conditions in their user instructions. The main concern is not a generally assumed movement, but heat production. Adjacent organs (brain, spine, joints) are deemed safe after three months following implantation of a stent. But be aware that many freestanding MRI facilities don't know this information. Therefore, carry the manufacturer's implant card with you, so that the MRI staff can look it up on the manufacturer's website or call the Stony Brook Heart Institute for guidance at (631) 44-HEART (444-3278).