The cardiac experts at Stony Brook Heart Institute are continually exploring new approaches to care for heart and valve disease patients, especially those too ill for open-heart surgery or those who might have limited treatment options.
In the latest chapter in Stony Brook’s state-of-the-art, minimally invasive frontline treatments, the Heart Institute has been selected to participate in the first-phase clinical trial for a new type of minimally invasive intravascular "patch" in advance of submission for approval by the U.S. Food and Drug Administration (FDA). Stony Brook is one of only five elite sites nationwide and the only facility on Long Island to be chosen to take part.
The fully absorbable intravascular "patch" is designed to seal an artery from the inside after heart valve repair or replacement. The flexible patch is roughly the size of a penny.
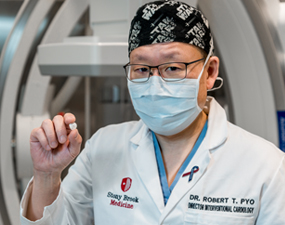
For the first time in the U.S., this new arterial-closing technique using PerQseal®+ was performed on March 8, 2022 by Henry J. Tannous, MD, and Robert T. Pyo, MD, at Stony Brook University Hospital during a transcatheter aortic valve procedure (TAVR).
Approved for use in Europe in 2018, the first generation of the device is a sutureless, fully-absorbable intravascular ‘patch’ that seals an artery from the inside after heart valve repair or replacement. The next generation of the device is designed to address more complex patient anatomies.
Looking Beyond Today's Answers
“Closing the artery has been a universal concern since less invasive techniques have been used for valve implantation,” said Robert T. Pyo, MD, Director, Interventional Cardiology; Medical Director, Structural Heart Program and Associate Professor, Renaissance School of Medicine at Stony Brook University. "To date, there has been no universally accepted way to close the implantation hole, whether applying pressure for up to two hours or utilizing a suture."
Exploring New Techniques to Enhance Safety
“Safe, quick and effective blood vessel closure is key to a successful outcome in patients undergoing an endovascular heart valve procedure,” says Henry J. Tannous, MD, Co-Director, Stony Brook Heart Institute; Chief, Cardiothoracic Surgery; Surgical Director, Structural Heart Program; and General T.F. Cheng Chair, Cardiothoracic Surgery, Renaissance School of Medicine at Stony Brook University. “At the Heart Institute, we are continually focused on exploring new options to improve outcomes and quality of life.”
Minimally invasive, lifesaving techniques for at-risk patients, which include utilizing the Impella® ventricular support system and transcatheter aortic valve replacement (TAVR), have soared in use over the past decade. These approaches, using compression or sutures to close the large-size percutaneous (through the skin) implantation holes, have not kept pace with the evolving technology. The intent of this type of minimally invasive intravascular "patch" is to fill that gap.

(L-R) Mia Wiedersum, RN; Julie Mangan, RN; interventional cardiologist Robert Pyo, MD; cardiothoracic surgeon Henry Tannous, MD; and interventional cardiologist, Ahmad Alkhalil, MD
Put Your Heart Health First
If you are at risk or if someone in your family has a heart condition, it’s important to schedule a visit with a cardiologist for preventive care. Our cardiologists can help you improve your heart health and/or prevent the progression of cardiovascular disease with a comprehensive heart disease risk assessment and treatment options.
Do something good for your own heart health by taking a free heart health assessment now.
For information and appointments
Call (631) 44-HEART (444-3278) or request an appointment online.

